Type 1 diabetes (T1D) is an autoimmune condition that affects millions worldwide. Unlike Type 2 diabetes, which is often linked to lifestyle factors, Type 1 diabetes is primarily caused by the body’s immune system mistakenly attacking insulin-producing beta cells in the pancreas. While the exact cause of T1D remains elusive, genetics play a significant role in determining who is at risk. Understanding how genetics influence T1D can help in early detection, management, and even potential prevention.
Understanding Genetics and Type 1 Diabetes
1. Genetic Risk Factors for Type 1 Diabetes
T1D has a strong genetic component, with certain gene mutations increasing an individual’s risk of developing the condition. The most well-known genetic predispositions are linked to the HLA (human leukocyte antigen) genes on chromosome 6, which regulate immune responses. Specific variants of these genes can increase the likelihood of the immune system mistakenly attacking beta cells.
- HLA-DR and HLA-DQ Genes: People with certain variants of these genes have a higher risk of developing T1D. These gene variants are responsible for triggering autoimmune reactions in genetically susceptible individuals.
- Other Genetic Mutations: In addition to HLA, other gene mutations such as INS (insulin gene) and PTPN22 (protein tyrosine phosphatase) have been linked to T1D. Mutations in these genes may contribute to how the immune system behaves and how beta cells function.
2. Family History and Type 1 Diabetes
While not all individuals with a family history of T1D will develop the condition, having a first-degree relative with T1D increases the risk. For example, if a parent or sibling has T1D, the risk of developing the disease increases by 15-20 times compared to the general population.
- Inherited Susceptibility: Inheriting the genetic mutations associated with T1D from one or both parents significantly increases the chances of developing the condition. However, environmental triggers, such as viral infections or certain dietary factors, are also necessary to initiate the autoimmune response.
3. Gene-Environment Interactions
Genetics alone cannot fully explain why some people develop T1D. Environmental factors play a crucial role in triggering the disease in genetically susceptible individuals. These factors include viral infections, toxins, and even certain dietary components during early childhood.
- Viral Triggers: Certain viruses, such as enteroviruses, are believed to trigger an immune response in genetically predisposed individuals, potentially leading to the onset of T1D.
- Environmental Influence: Other environmental elements, such as early introduction to cow’s milk, lack of breastfeeding, or low vitamin D levels, have also been studied as potential risk factors for T1D in genetically susceptible individuals.
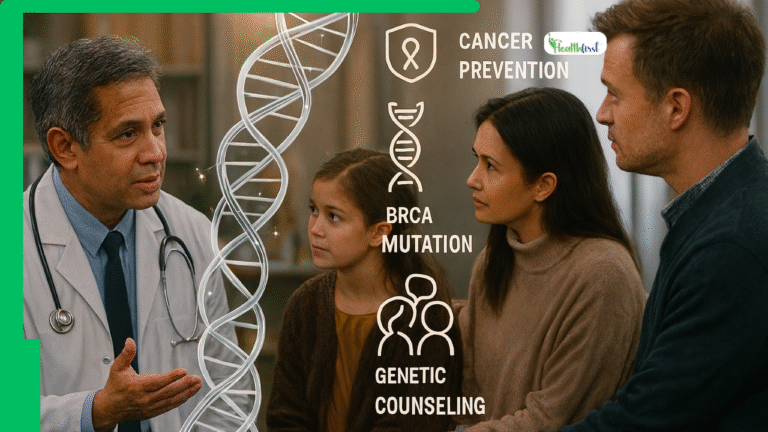
4. Preventive Research: Genetic Screening
With advancements in genetic research, screening for T1D risk has become more feasible. Individuals with a family history of T1D or those carrying specific gene variants can undergo genetic testing to assess their risk. Early identification allows for close monitoring and the possibility of early interventions.
- Research in Immunotherapy: Studies are ongoing in immunotherapy treatments aimed at altering the immune response in at-risk individuals to prevent the onset of T1D before symptoms appear. These treatments hold promise for delaying or even stopping the autoimmune process in genetically predisposed individuals.
Conclusion: Genetics and the Future of Type 1 Diabetes Care
Understanding the role of genetics in Type 1 diabetes is key to future prevention and treatment strategies. While genetics cannot be changed, advancements in genetic research and precision medicine are making it possible to identify those at risk earlier and offer targeted interventions. This knowledge can improve outcomes and potentially delay or prevent the onset of T1D in future generations.